Overactive Bladder Syndrome (OAB)
Overactive bladder (OAB) is a treatable condition where the bladder muscles contract unpredictably, creating disruptive urinary symptoms. While causes range from neurological factors to lifestyle triggers, OAB is not an inevitable part of aging. With 30% of adults affected, it’s more common in women and older men with prostate health issues. A urologist can diagnose OAB through tests and a bladder diary, offering personalized solutions from behavioral changes to advanced therapies.
What is an Overactive Bladder?
Overactive bladder (OAB) is a condition characterized by a sudden, uncontrollable urge to urinate. This bladder overactivity can disrupt daily life and lead to frequent trips to the bathroom, even at night.
Common Symptoms of Overactive Bladder
- Urinary urgency: A strong, sudden need to urinate that’s hard to ignore.
- Urinary frequency: Needing to urinate more than 8 times in 24 hours.
- Nocturia: Waking up multiple times at night to urinate.
- Urge incontinence: Leaking urine when you can’t reach a toilet in time.
OAB affects about 30% of adults, with higher prevalence in women. Among men over 70, 50% experience symptoms, often linked to prostate enlargement.
OAB occurs when bladder muscles contract involuntarily, creating urgency even with little urine. While the exact cause is often unknown (idiopathic), contributing factors include:
- Neurological conditions: Stroke, Parkinson’s disease, or diabetes.
- Bladder abnormalities: Infections, stones, or obstructions (e.g., enlarged prostate).
- Lifestyle factors: Excess caffeine, alcohol, or fluid intake.
- Aging: A risk factor, but OAB is not a normal part of aging.
Your urologist will conduct:
- Medical history and physical exam.
- Urine tests (analysis, culture).
- Bladder ultrasound or uroflowmetry.
- Bladder diary: A 3-day log of fluid intake, urination frequency, and leaks.
- Urodynamic studies (if needed): Measures bladder pressure and function (minimal discomfort).
Your Bladder Diary: A Helpful Tracking Tool
![]()
A bladder diary is a simple way to record your urinary patterns to help your urologist understand your symptoms better. Your Bladder Diary_A Helpful Tracking Tool. Here’s what you’ll track:
- Fluid intake: What and how much you drink
- Bathroom visits: When and how often you urinate (day and night)
- Urine volume: How much you pass each time (optional)
- Leak episodes: Any accidental urine loss
Why it matters:
• Reveals patterns in your symptoms
• Helps identify potential triggers
• Guides your personalized treatment plan
Tracking tips:
✓ Record for 3 full days (including 2 weekdays + 1 weekend day)
✓ Note times and approximate amounts
✓ Include any symptoms or leaks
This easy-to-use diary provides valuable insights that office tests can’t capture, helping your doctor recommend the most effective treatment options for you.
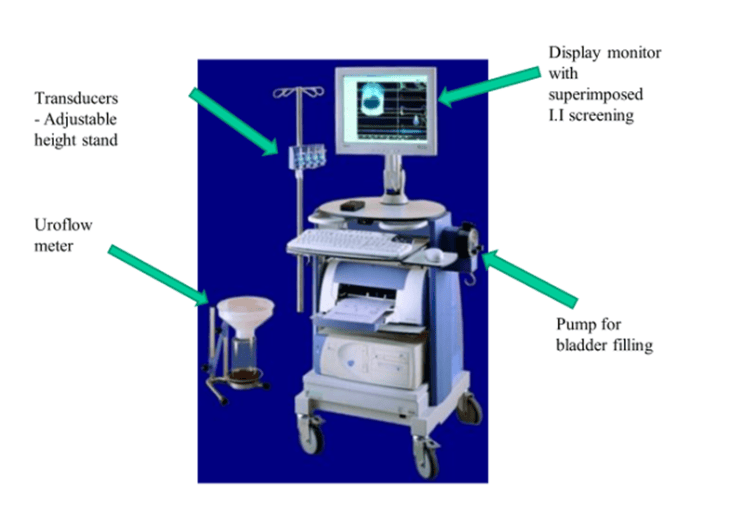
A urodynamic study helps your urologist evaluate how well your bladder and urethra are functioning. During this test:
- We gently fill your bladder with sterile fluid to measure its response
- Special sensors record pressure changes in your bladder muscles
- The test provides precise data about your bladder’s capacity and emptying ability
Will it hurt?
Most patients experience only mild discomfort during the procedure. You may feel:
- A temporary sensation when the small sensors are placed
- Pressure as your bladder fills
- The urge to urinate during testing
While not painful, some find the experience slightly awkward. Our team will guide you through each step to ensure your comfort. The entire process typically takes 30-45 minutes, and you can resume normal activities afterward.
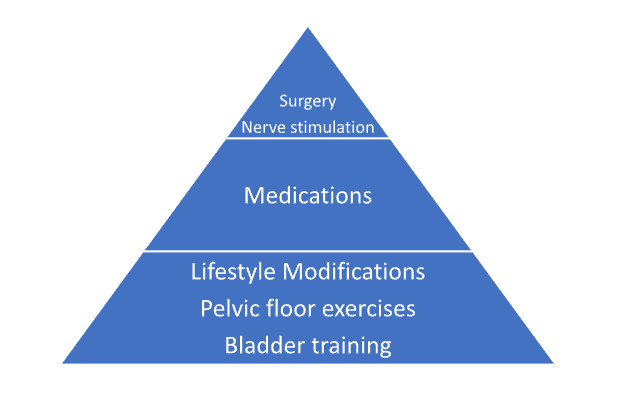
1. Lifestyle Modifications & Bladder Training
For less severe symptoms, this initial approach is tailored to your voiding diary. It includes;
- Bladder training: Gradually delaying urination and using deep breathing techniques to manage urgency
- Diet adjustments: Limiting fluids before bedtime and reducing caffeine/alcohol
- Pelvic floor exercises: Strengthening muscles to improve control
- Biofeedback: Using sensors to better understand bladder function
2. Medications
- Anticholinergics (e.g., Oxybutynin, Tolterodine, Solifenacin): These medications block nerve signals that trigger involuntary bladder contractions, helping reduce urgency and frequency.
- Mirabegron: A newer option that relaxes the bladder muscle to improve control.
Possible side effects: Dry mouth, dry eyes, or constipation may occur with anticholinergics. Mirabegron typically has fewer side effects.
3. Nerve Stimulation
This gentle therapy uses a thin needle placed near your ankle to deliver mild electrical signals to nerves that control bladder function. The treatment:
- Is performed in a doctor’s office (no hospital stay needed)
- Takes about 30 minutes per session
- Typically involves weekly treatments for 12 weeks
- May cause temporary mild tingling but is generally not painful
Most patients can resume normal activities immediately after each session. Many notice gradual improvement in bladder control as treatment progresses.
4. Botox® Injections
For patients who continue to experience symptoms despite trying other treatments, Botox® injections offer an effective solution. During this minimally invasive procedure:
- A urologist uses a thin scope (cystoscope) to place Botox® directly into the bladder wall
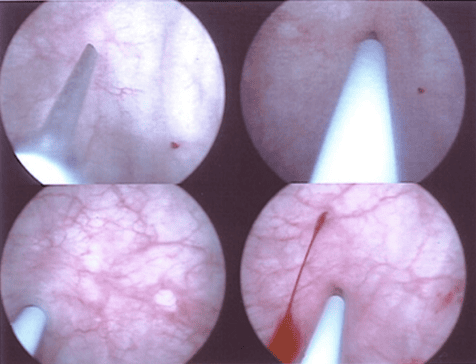
Intravesical injection of Botulinum toxin
- The treatment helps calm overactive bladder muscles
- Results typically last 6-12 months before needing a repeat treatment
Most patients experience:



The procedure is performed in-office and takes about 15-30 minutes. While the effects are temporary, many patients find the lasting relief well worth repeating the treatment as needed.
Request an Appointment
FAQs About Overactive Bladder
No. While aging increases risk, OAB is a medical condition with treatable causes.
Yes. Caffeine, alcohol, and acidic foods can worsen urinary urgency and frequency.
Very. Strengthening pelvic muscles improves urge incontinence control for many patients.
UTIs cause burning/pain; OAB involves bladder overactivity without infection. Testing confirms the cause.
If symptoms disrupt daily life or lifestyle changes don’t help, seek evaluation to rule out underlying issues.