Male Infertility – Is There Help?
To better understand your symptoms, visit us for a comprehensive diagnosis and personalised treatment plan
Male Infertility – Is There Help?
What is male infertility? How common is this problem?
Male infertility describes the condition where men are unable to cause successful pregnancy in their fertile female partners. 1 in 5 couples attempting to conceive a child will be unsuccessful after deliberately trying for a year or more. Of these unsuccessful couples, male infertility accounts for up to 2/3 of all cases. Understandably, this causes much anguish and distress for the couple and their family members.
For successful natural conception to occur, the male partner must be able to (1) produce healthy motile sperm in adequate numbers; (2) be able to perform penetrative sexual intercourse with his female partner during her ovulatory period; and (3) the sperm must be successfully ejaculated into the female vagina during climax, and successfully swim up the female genital tract to unite with the ovum, creating a fertilized ovum that (over the course of 8-9 days) will implant in the female’s womb, where it will mature over 9 months.
Common causes for male infertility include:
A. Poor sperm production and quality
• Impaired hormone production by the brain’s pituitary gland
• Advanced age
• Obesity
• Drugs, tobacco and alcohol
• Chemotherapy
• Previous infection, cancer or trauma to the testicles
• Previous maldescent of the testicles in early childhood
• Dilatation of the testicular veins near the testis (varicocele)
B. Difficulties with successful ejaculation of sperm
• Congenital absence of the vas deferens (tubes carrying sperm away from testicles)
• Blockage of the ejaculatory ducts
• Infection of the prostate
• Erectile dysfunction (inability to start or maintain an erection)
• Previous vasectomy (surgical ligation of the tubes carrying sperm away from testicles)
When you consult your urologist, he will usually ask you a detailed medical history to identify possible medical causes. He will then perform a physical examination to assess the male genitals, and use ultrasonography to assess the testicles, prostate and seminal vesicles. He will then order a series of blood tests to assess your general health, testosterone and hormone profile. He will also request a semen sample for laboratory analysis. The volume of the semen sample, number of total sperm cells, sperm motility/forward progression, and percentage of sperm with normal morphology are measured (Fig.1).
Illustration
Figure 1: In semen analysis, the number of sperm, their morphology and motility are assessed quantitatively.
That depends on the cause and severity of the problem. General measures that will help improve the health and quality of the male’s sperm include stopping tobacco smoking; reducing alcohol intake; reducing excess body weight through regular sustained exercise; and avoiding heat or trauma to the testicles, such as saunas. Frequency of ejaculation is also important, as prolonged abstinence > 2 weeks also impairs sperm quality.
In men with low testosterone levels, this can be easily treated with medications. Various supplements eg. Vitamin E, Co-enzyme Q10, arginine, lycopene etc have also been reported to improve sperm counts and quality. For men with varicoceles, surgical ligation of these dilated testicular veins (varicocelectomy) reduces sperm DNA damage and seminal oxidative stress, and improves sperm morphology. Around 70% of patients demonstrate improved sperm quality after varicocelectomy, and increases successful conception in about 40% of patients. This surgery is a simple day surgery procedure usually performed with the assistance of the operating microscope, with few side effects (Fig. 2).
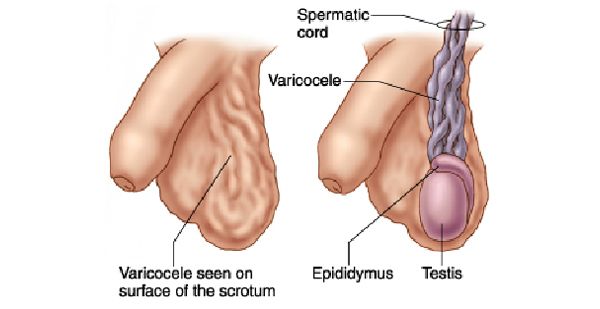
Illustration
Figure 2: During varicocelectomy, the dilated testicular veins are cut and the ends ligated.
For some men with previous vasectomy wishing to father children due to change of circumstances (unexpected bereavement of their children, divorce and wishes of a new partner to start a new family, etc), microsurgical reversal of vasectomy with is an option. The success of these reversal procedures, as evidenced by the presence of sperm in the ejaculate, has been reported in 85-90% of men. However, only about 60% of couples actually go on to successfully conceive a baby after vasovasostomy. Female partners who are over the age of 35 years and have not borne children before, are less likely to result in successful pregnancy despite a successful vasectomy reversal.
If patients with male infertility still fail to achieve successful pregnancy with their partners despite the above measures the couple will need to consider forms of assisted reproduction. This could be in a variety of ways, and will involve harvesting and processing healthy sperm either from a semen sample, or directly from the testicles under anaesthesia.
A. Intrauterine insemination (IUI):
A small tube is used to inject processed sperm through the female cervix into the female’s womb. By bypassing the cervical mucus, more motile sperm can reach the Fallopian tubes where normal fertilization can occur (Fig. 3).
Illustration
Figure 3: Illustration of intrauterine insemination (IUI), showing how the processed sperm is delivered through a catheter into the female’s womb.
B. In vitro fertilization (IVF):
In IVF, the ovaries of the female partners are hyperstimulated to cause several eggs (oocytes) to mature. Before ovulation occurs, these eggs are harvested with the aid of ultrasound guidance, and then mixed in the laboratory with processed sperm from the male partner. When fertilization occurs, the embryos are inserted back into the female’s womb. However, only 20-30% of replaced embroyos survive and become successful pregnancies. Around 15-18% of couples who fail IVF on the first cycle will be successful the second time round.
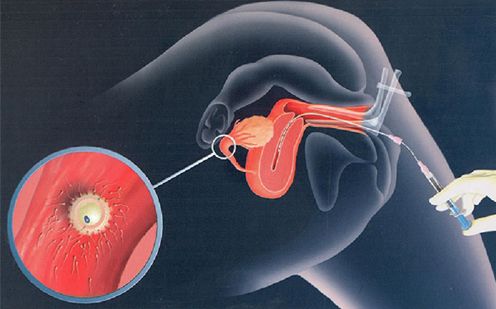
C. IVF with intracytoplasmic sperm injection (IVF-ICSI):
This approach is the most popular for addressing male factor infertility. By injecting a single healthy sperm directly into an oocyte under microscope guidance (Fig. 4), multiple natural barriers to fertilization are bypassed, and pregnancy success rates are greatly improved (40-50%) when compared to conventional IVF (20-30%). Children born through IVF-ICSI do not demonstrate any increased risk of birth or developmental defects. However, around 1 in 3 pregnancies achieved with IVF-ICSI result in multiple gestations (twins or triplets), which may be a challenge for some couples.

Illustration
Figure 4: IVF-ICSI, where a single healthy sperm is delivered directly into an oocyte under microscopic guidance.
- 1 in 5 couples will have difficulty conceiving children, and male infertility accounts for up to 2/3 of all affected couples
- Couples who fail to conceive after a year of deliberate attempts should consult their gynaecologist or urologist for assessment of possible treatable causes
- Advances in assisted reproduction techniques now offer new hope for previously infertile couples – the most appropriate technique depends on the cause and the couple’s expectations
